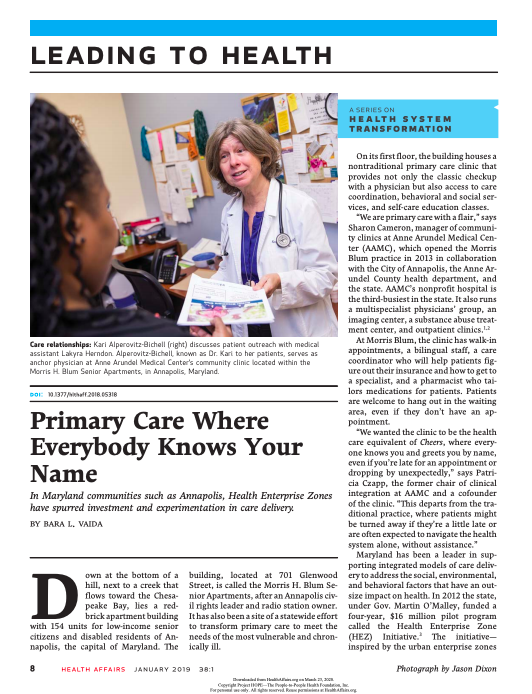
This article details how Maryland has been a leader in supporting integrated models of care delivery to address the social, environmental, and behavioral factors that have an outsize impact on health.
In 2012, the state funded a four-year, $16 million pilot program called the Health Enterprise Zone (HEZ) Initiative. The initiative—inspired by the urban enterprise zones intended to increase economic development in low-income communities—provided a mix of tax credits and grants to five underserved zones in the state to encourage health providers and community leaders to work together to improve health outcomes and save money.
Between 2013 and 2016, communities with an HEZ reduced inpatient admissions at Maryland hospitals and saved the state’s health system about $93.4 million. Residents in the zones reported that they had become more aware of their health and were exercising more and monitoring their diets. Providers said that the HEZs helped patients manage their chronic conditions.
Beginning in 2019, Maryland primary care doctors have had the option to join in the state’s all-payer Total Cost of Care Model for Medicare beneficiaries, dubbed the global budget. Providers who participate in the model can make more money if their Medicare patients are healthier. The global budget, which already caps the amount of money hospitals can receive for Medicare patients, has been in place in Maryland since 2014. Maryland has had a waiver from the Centers for Medicare and Medicaid Services since the mid-1970s that enables it to set rates for hospital services.
This article is part of a series on transforming health systems published with support from the Robert Wood Johnson Foundation.
 Back to Resources
Back to Resources